Vertical Nystagmus: An In-depth Exploration of Involuntary Vertical Eye Movements
Vertical nystagmus represents one of the most diagnostically significant forms of involuntary eye movement disorders. Unlike horizontal nystagmus, which can have various benign causes, vertical nystagmus often signals serious underlying neurological pathology requiring immediate attention. This comprehensive analysis explores the complex mechanisms, critical diagnostic implications, and evolving treatment strategies for vertical nystagmus based on current neurological research and clinical evidence.
Anatomy of Abnormal Vertical Eye Movements
Understanding vertical nystagmus requires a detailed knowledge of the neural pathways controlling vertical eye movements. The vertical gaze system involves multiple interconnected brain regions working in precise coordination to maintain stable vertical eye positioning.
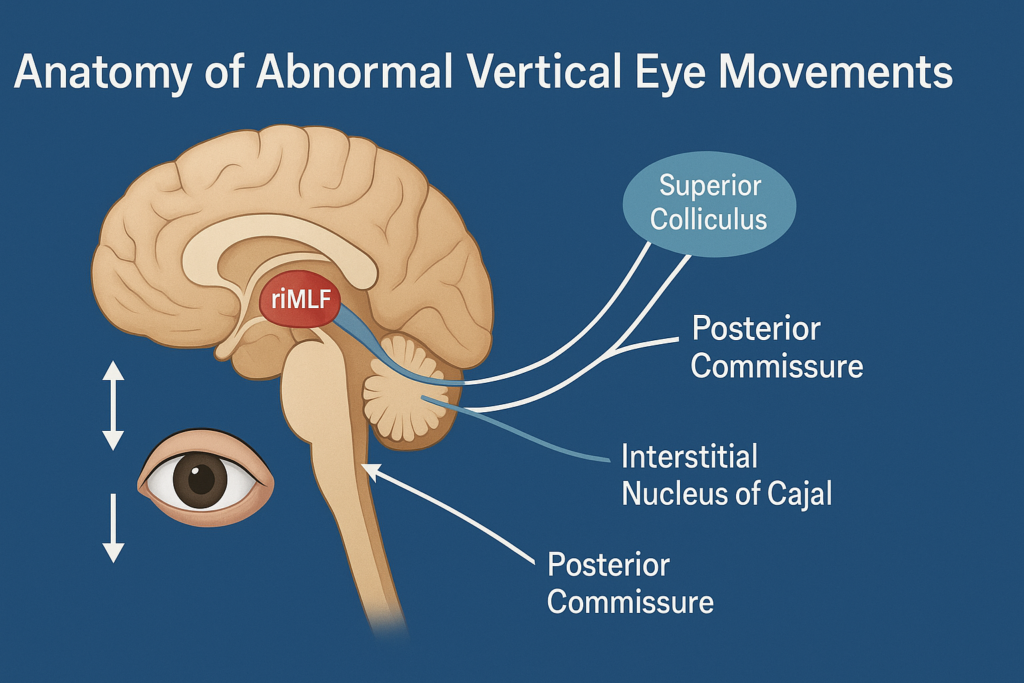
The primary neural structures controlling vertical eye movements include:
- Rostral Interstitial Nucleus of the Medial Longitudinal Fasciculus (riMLF): This critical brainstem nucleus serves as the primary burst generator for vertical saccades and is essential for maintaining vertical gaze stability.
- Interstitial Nucleus of Cajal (INC): Functions as the neural integrator for vertical eye movements, converting velocity signals into position signals to maintain stable vertical gaze.
- Posterior Commissure: Connects the bilateral vertical gaze centers and is crucial for coordinating symmetric vertical eye movements.
- Superior Colliculus: Contributes to vertical saccade generation and integrates visual and spatial information for accurate vertical targeting.
When these structures are damaged or dysfunctional, the result is often vertical nystagmus with characteristic patterns that can provide crucial diagnostic information about the location and nature of the underlying pathology.
According to research published in the Journal of Neuro-Ophthalmology, vertical nystagmus patterns can be precisely mapped to specific anatomical lesions, making them invaluable diagnostic tools for neurologists and neuro-ophthalmologists.
Specific Forms of Vertical Nystagmus: Upbeat and Downbeat
Vertical nystagmus manifests in two primary forms, each with distinct clinical implications and underlying mechanisms:
Upbeat Nystagmus
Upbeat nystagmus is characterized by the fast phase of the nystagmus beating upward. This form is typically associated with lesions in the lower brainstem, particularly affecting:
- Medullary Tegmentum: Damage to this region, often from stroke or demyelinating disease, disrupts the normal inhibitory influences on upward eye movements.
- Inferior Cerebellar Vermis: Lesions in this area, including tumors or degenerative conditions, can produce upbeat nystagmus by affecting the cerebellum’s modulatory influence on vertical gaze.
- Cerebellopontine Angle: Masses or inflammatory conditions in this region may compress critical neural pathways, resulting in upbeat nystagmus.
Clinical studies documented in Brain demonstrate that upbeat nystagmus often occurs in conjunction with other brainstem signs, including ataxia, dysarthria, and cranial nerve palsies.
Downbeat Nystagmus
Downbeat nystagmus is perhaps the most clinically significant form of vertical nystagmus, as it almost invariably indicates serious central nervous system pathology. The fast phase beats downward, and the condition is associated with:
- Cervicomedullary Junction Abnormalities:
- Arnold-Chiari malformations are the most common structural cause
- Basilar invagination and other craniocervical junction anomalies
- Syringobulbia affecting the medullary tegmentum
- Cerebellar Flocculus Dysfunction: The flocculus normally provides inhibitory input to prevent unwanted downward drift of the eyes. When damaged, this results in the characteristic downbeat pattern.
- Drug-Induced Causes: Certain medications, particularly anticonvulsants like phenytoin and lithium, can cause reversible downbeat nystagmus through their effects on cerebellar function.
- Metabolic Disorders: Thiamine deficiency, magnesium depletion, and other metabolic disturbances can manifest as downbeat nystagmus.
Research from the American Journal of Ophthalmology indicates that downbeat nystagmus patients often experience severe visual symptoms and balance problems, making early diagnosis and treatment crucial for preventing falls and maintaining quality of life.
Neurological Implications of Vertical Nystagmus
The presence of vertical nystagmus carries profound neurological implications that extend far beyond simple eye movement abnormalities:
Diagnostic Red Flags
Vertical nystagmus should be considered a neurological emergency requiring immediate evaluation when accompanied by:
- Acute Onset with Severe Headache: May indicate posterior circulation stroke, particularly involving the vertebrobasilar system.
- Progressive Neurological Symptoms: Including difficulty swallowing, speech changes, or limb weakness, suggesting expanding lesions like tumors or inflammatory conditions.
- Signs of Increased Intracranial Pressure: Such as papilledema, altered consciousness, or vomiting, which may indicate hydrocephalus or mass effect.
Associated Neurological Syndromes
Vertical nystagmus frequently occurs as part of broader neurological syndromes:
- Wallenberg Syndrome (Lateral Medullary Syndrome): Often presents with vertical nystagmus along with facial sensory loss, ataxia, and swallowing difficulties.
- Dorsal Midbrain Syndrome (Parinaud’s Syndrome): Characterized by upward gaze palsy, pupillary abnormalities, and convergence-retraction nystagmus.
- Cerebellar Degeneration Syndromes: Progressive conditions like spinocerebellar ataxias often manifest early with vertical nystagmus before other symptoms become apparent.
Studies published in Movement Disorders emphasize that recognizing these patterns early can lead to more timely intervention and better patient outcomes.
Diagnostic Journey to Identify Vertical Nystagmus
The diagnostic approach to vertical nystagmus requires systematic evaluation combining clinical assessment with advanced investigative techniques:
Initial Clinical Assessment
- Comprehensive History Taking:
- Timeline of symptom onset (acute vs. gradual)
- Associated symptoms (headache, balance problems, hearing changes)
- Medication history (particularly anticonvulsants and psychotropic drugs)
- Family history of neurological conditions
- Detailed Neurological Examination:
- Complete cranial nerve assessment
- Coordination and balance testing
- Assessment of gait and station
- Fundoscopic examination for papilledema
- Specialized Ocular Motor Testing:
- Documentation of nystagmus characteristics (amplitude, frequency, direction)
- Assessment of other eye movement abnormalities
- Testing for positional variations in nystagmus intensity
Advanced Diagnostic Techniques
- Video-Oculography (VOG): High-resolution recording of eye movements allows precise characterization of nystagmus patterns and quantification of improvement with treatment.
- Magnetic Resonance Imaging (MRI):
- High-resolution imaging of the brainstem and cerebellum
- Special attention to the craniocervical junction
- Gadolinium enhancement to identify inflammatory or neoplastic processes
- Magnetic Resonance Angiography (MRA): Evaluation of posterior circulation vessels to identify vascular causes of brainstem dysfunction.
- Lumbar Puncture: When inflammatory conditions are suspected, cerebrospinal fluid analysis can provide crucial diagnostic information.
- Metabolic and Nutritional Assessment: Blood tests for thiamine, magnesium, B12, and other vitamins that may contribute to vertical nystagmus.
Research from Clinical Neurophysiology demonstrates that combining multiple diagnostic modalities increases diagnostic accuracy and helps guide appropriate treatment decisions.
Specialized Therapeutic Approaches
Treatment of vertical nystagmus focuses on addressing both the underlying cause and managing symptomatic relief:
Cause-Specific Treatments
- Surgical Interventions:
- Chiari decompression for Arnold-Chiari malformations
- Tumor resection when space-occupying lesions are identified
- Ventriculoperitoneal shunting for hydrocephalus
- Medical Management of Underlying Conditions:
- Immunosuppressive therapy for inflammatory conditions
- Vitamin supplementation for nutritional deficiencies
- Medication adjustment when drug-induced causes are identified
Symptomatic Treatments
- Pharmacological Approaches:
- 4-Aminopyridine (4-AP): Research published in Neurology shows significant efficacy in treating downbeat nystagmus, with many patients experiencing substantial improvement in both nystagmus intensity and functional vision.
- Baclofen: Particularly effective for periodic alternating nystagmus and some forms of vertical nystagmus
- Gabapentin: Has shown promise in reducing nystagmus amplitude and improving visual symptoms
- Memantine: An NMDA receptor antagonist that may help stabilize eye movements
- Optical Interventions:
- Base-down prisms: Can help patients with downbeat nystagmus by moving images into their area of better visual stability
- Specialized contact lenses: May provide proprioceptive feedback that helps dampen nystagmus
- Tinted lenses: Reduce light sensitivity often associated with vertical nystagmus
- Physical Rehabilitation:
- Vestibular rehabilitation therapy: Customized exercises to improve balance and reduce fall risk
- Gaze stabilization exercises: Help patients develop compensatory strategies for maintaining visual focus
- Balance training: Particularly important given the high fall risk in patients with vertical nystagmus
Emerging Therapeutic Modalities
- Transcranial Stimulation: Early research suggests that transcranial direct current stimulation (tDCS) targeting cerebellar regions may help modulate vertical nystagmus.
- Botulinum Toxin Injections: Limited studies have explored botulinum toxin injections into extraocular muscles as a potential treatment for severe vertical nystagmus.
- Gene Therapy Research: For rare genetic causes of vertical nystagmus, targeted gene therapies are under investigation, though these remain in preclinical stages.
Living with Vertical Nystagmus: Challenges and Strategies
Managing daily life with vertical nystagmus presents unique challenges that require comprehensive adaptive strategies:
Visual Function Optimization
- Environmental Modifications:
- Improved lighting to reduce visual strain
- High-contrast markings for stairs and edges
- Reduction of visual clutter in frequently used spaces
- Reading and Near Work Adaptations:
- Large print materials and magnification devices
- Electronic reading devices with adjustable font sizes
- Proper positioning to minimize nystagmus during reading tasks
- Technology Integration:
- Screen readers and voice-to-text software
- Smartphone apps designed for visual impairment
- GPS navigation systems with audio guidance
Safety Considerations
- Fall Prevention: Given the significant balance impairments often associated with vertical nystagmus, comprehensive fall prevention strategies are essential:
- Home safety assessments and modifications
- Physical therapy focused on balance and coordination
- Appropriate use of mobility aids when necessary
- Driving Considerations: Many patients with vertical nystagmus face restrictions or complete inability to drive safely. Occupational therapy evaluations can help determine individual capabilities and limitations.
Psychosocial Support
The impact of vertical nystagmus extends beyond physical symptoms:
- Counseling and Support Groups: Connecting with others who have similar conditions can provide emotional support and practical advice.
- Occupational Adaptations: Working with vocational rehabilitation specialists to modify work environments or explore alternative career paths.
- Educational Support: For students, coordination with educational professionals to ensure appropriate accommodations and support services.
Studies from Quality of Life Research emphasize that comprehensive support addressing both medical and psychosocial needs leads to better overall outcomes for patients with vertical nystagmus.
Frequently Asked Questions About Vertical Nystagmus
Is vertical nystagmus always a sign of serious disease?
While vertical nystagmus is more likely to indicate significant neurological pathology compared to horizontal nystagmus, not all cases represent immediately life-threatening conditions. However, all instances of vertical nystagmus warrant prompt neurological evaluation to rule out treatable causes.
Can vertical nystagmus be completely cured?
The prognosis for vertical nystagmus depends entirely on the underlying cause. Some causes, such as drug-induced nystagmus or nutritional deficiencies, may be completely reversible with appropriate treatment. Structural causes like Chiari malformation may improve significantly with surgical intervention, while degenerative conditions may require ongoing symptomatic management.
How quickly should someone with new-onset vertical nystagmus seek medical attention?
New-onset vertical nystagmus, particularly when accompanied by other neurological symptoms, should be evaluated emergently. Even when occurring in isolation, vertical nystagmus warrants urgent neurological assessment within 24-48 hours of onset.
Are there any activities that should be avoided with vertical nystagmus?
Safety considerations are paramount. Activities requiring precise visual-motor coordination, such as driving, operating heavy machinery, or working at heights, may need to be modified or avoided depending on the severity of symptoms. Each individual should work with their healthcare team to determine appropriate activity restrictions.
Can children develop vertical nystagmus?
While less common in children than adults, vertical nystagmus can occur in pediatric populations. When present, it often indicates serious underlying conditions such as brain tumors, genetic disorders, or developmental abnormalities. Prompt pediatric neurological evaluation is essential.
Conclusion: Navigating the Complex Landscape of Vertical Nystagmus
Vertical nystagmus represents a critical intersection between ophthalmology and neurology, demanding comprehensive evaluation and multidisciplinary management. Unlike other forms of nystagmus that may have benign causes, vertical nystagmus serves as an important neurological warning sign that should never be ignored.
Recent advances in neuroimaging, pharmacological treatments, and rehabilitation techniques have significantly improved outcomes for patients with vertical nystagmus. The development of targeted therapies like 4-aminopyridine has provided new hope for symptomatic relief, while improved diagnostic techniques allow for earlier identification and treatment of underlying causes.
The key to successful management lies in prompt recognition, thorough evaluation, and individualized treatment approaches that address both the underlying pathology and the functional impact of the condition. As our understanding of the neural mechanisms underlying vertical eye movement control continues to advance, even more effective treatments are likely to emerge.
For individuals experiencing symptoms suggestive of vertical nystagmus, immediate consultation with a neurologist or neuro-ophthalmologist is essential. Early intervention can often prevent progression of underlying conditions and significantly improve long-term outcomes.
Understanding the relationship between vertical nystagmus and related conditions such as vertigo and nystagmus can provide additional context for patients and their families navigating this complex condition. Additionally, awareness of comprehensive diagnostic approaches can help ensure thorough evaluation and appropriate treatment planning.
This article represents current medical understanding of vertical nystagmus based on peer-reviewed research and clinical guidelines. Individual cases may vary, and this information should not replace personalized medical advice from qualified healthcare professionals.