Rotational Nystagmus: Demystifying Circular Eye Movements
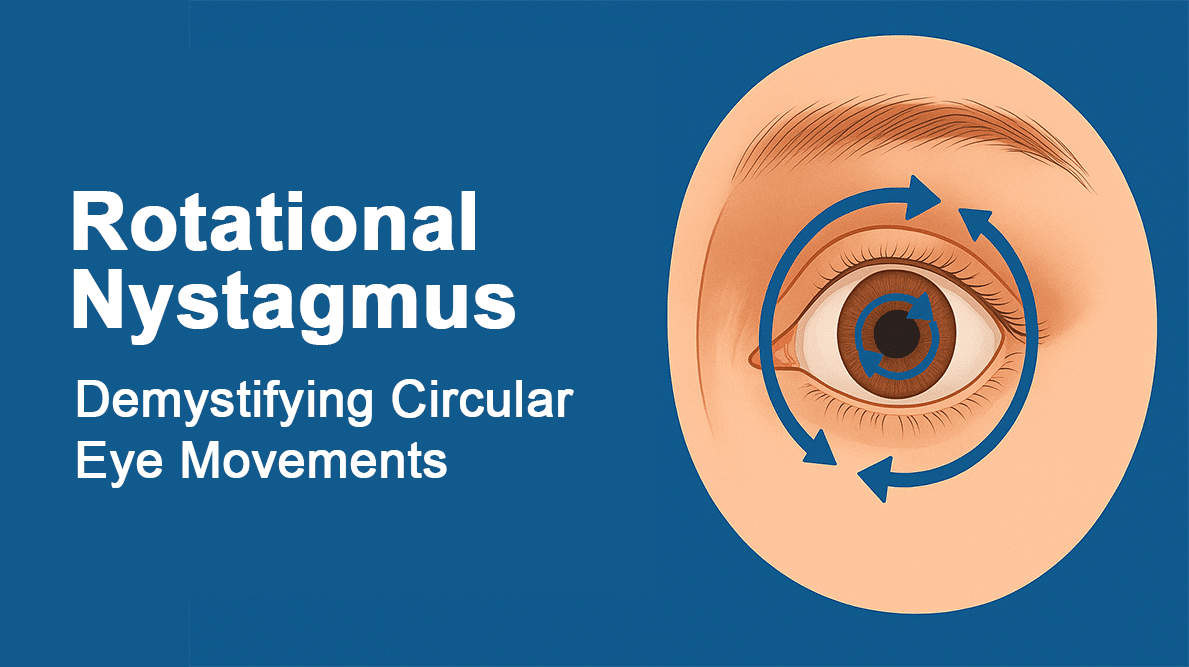
Rotational nystagmus, also known as torsional or rotatory nystagmus, represents one of the most complex and diagnostically challenging forms of involuntary eye movement disorders. Characterized by circular or wheel-like oscillations around the visual axis, this condition often provides crucial diagnostic clues about underlying vestibular and neurological pathology. This comprehensive exploration delves into the intricate mechanisms, diagnostic significance, and evolving treatment strategies for rotational nystagmus based on current medical research and clinical expertise.
Unique Characteristics of Rotational Nystagmus
Rotational nystagmus distinguishes itself from other forms of involuntary eye movements through its distinctive circular motion pattern. Unlike the linear movements seen in horizontal or vertical nystagmus, rotational nystagmus involves clockwise or counterclockwise rotation of the eyes around their anteroposterior axis.
The biomechanics of rotational eye movements involve complex coordination of all six extraocular muscles working in precise synchronization. This intricate muscle coordination is controlled by specialized neural circuits in the brainstem that integrate vestibular, visual, and proprioceptive inputs to maintain rotational stability of the eyes.
Key characteristics that define rotational nystagmus include:
- Rotational Component: The primary movement occurs around the visual axis, creating a spinning or circular motion
- Mixed Patterns: Often combined with horizontal or vertical components, creating complex three-dimensional eye movements
- Vestibular Association: Frequently linked to disorders of the vestibular system, particularly the semicircular canals
- Diagnostic Significance: The presence and pattern of rotational nystagmus can provide specific information about the location and nature of underlying pathology
Research published in the Annals of Neurology demonstrates that rotational nystagmus patterns can be precisely correlated with specific anatomical lesions, making them invaluable diagnostic markers in neuro-otological evaluation.
How the Vestibular System Influences Rotational Movements
The vestibular system plays a fundamental role in generating and controlling rotational eye movements through the vestibulo-ocular reflex (VOR). Understanding this complex relationship is crucial for comprehending the pathophysiology of rotational nystagmus.
Semicircular Canal Function
The three semicircular canals in each inner ear—horizontal, anterior, and posterior—detect rotational head movements in three-dimensional space:
- Horizontal Semicircular Canals: Detect rotation around the vertical axis (head turning left or right)
- Anterior Semicircular Canals: Detect rotation in the sagittal plane (head nodding forward or backward)
- Posterior Semicircular Canals: Detect rotation in the coronal plane (head tilting side to side)
When these canals are stimulated by head movement or pathologically activated by disease, they generate compensatory eye movements designed to maintain visual stability. Dysfunction in any of these canals can result in abnormal rotational eye movements characteristic of rotational nystagmus.
Neural Pathways and Integration
The vestibular nuclei in the brainstem serve as the primary integration center for rotational eye movement control:
- Superior Vestibular Nucleus: Processes input from the horizontal and anterior semicircular canals
- Lateral Vestibular Nucleus: Primarily involved in postural control but also contributes to eye movement coordination
- Medial Vestibular Nucleus: Integrates signals from all semicircular canals and projects to ocular motor nuclei
- Inferior Vestibular Nucleus: Processes input from the posterior semicircular canal and otolith organs
Disruption at any level of this complex pathway can result in abnormal rotational eye movements. Studies from the Journal of Vestibular Research show that the specific pattern of rotational nystagmus can help localize the site of lesion within the vestibular pathway.
Associated Brain and Brainstem Pathologies
Rotational nystagmus can arise from various pathological conditions affecting different levels of the nervous system:
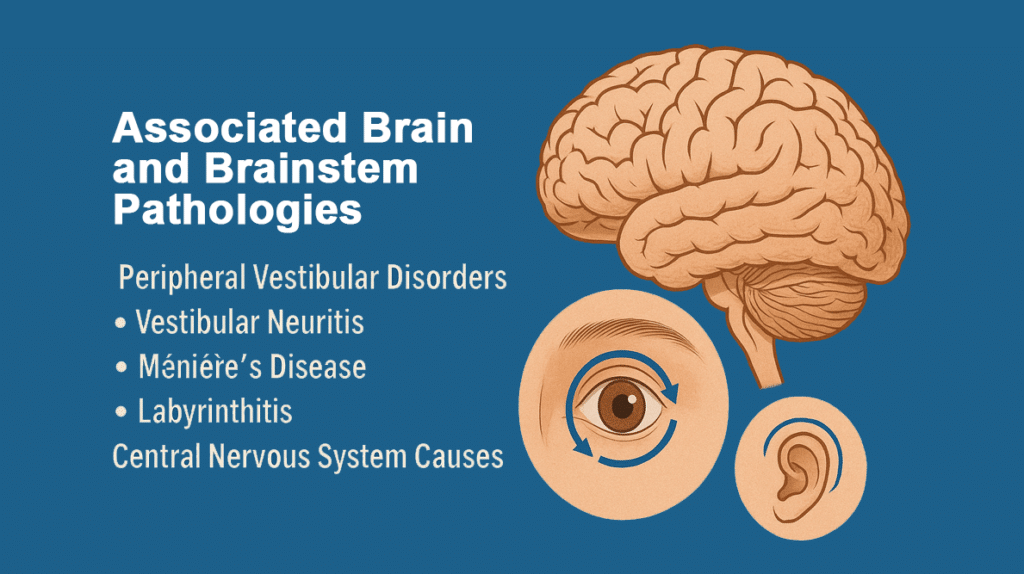
Peripheral Vestibular Disorders
- Benign Paroxysmal Positional Vertigo (BPPV):
- Posterior canal BPPV often produces rotatory-vertical nystagmus
- Horizontal canal BPPV may show rotational components along with horizontal movements
- The Dix-Hallpike maneuver characteristically triggers rotational nystagmus in posterior canal BPPV
- Vestibular Neuritis: Acute inflammation of the vestibular nerve can produce complex rotational nystagmus patterns, often with a mixed horizontal-rotational component that changes with head position.
- Ménière’s Disease: During acute attacks, patients may exhibit rotational nystagmus accompanied by severe vertigo, hearing loss, and tinnitus.
- Labyrinthitis: Inflammation of the inner ear structures can produce various patterns of rotational nystagmus depending on which semicircular canals are affected.
Central Nervous System Causes
- Cerebellar Pathology:
- Tumors affecting the cerebellopontine angle
- Cerebellar infarction or hemorrhage
- Degenerative cerebellar diseases like spinocerebellar ataxias
- Cerebellar lesions often produce complex rotational nystagmus patterns combined with other ocular motor abnormalities
- Brainstem Lesions:
- Multiple sclerosis plaques affecting vestibular nuclei
- Brainstem strokes involving the medulla or pons
- Tumors compressing brainstem structures
- Syringobulbia affecting central vestibular pathways
- Migraine-Associated Rotational Nystagmus: Vestibular migraine can produce episodic rotational nystagmus, often accompanied by typical migraine symptoms.
- Arnold-Chiari Malformation: This structural abnormality of the cerebellum and brainstem can produce various nystagmus patterns, including rotational forms.
Research from Brain indicates that the specific characteristics of rotational nystagmus—including direction, amplitude, and associated symptoms—can help differentiate between peripheral and central causes, guiding appropriate diagnostic workup and treatment decisions.
Advanced Imaging Techniques to Identify Causes
Modern diagnostic imaging has revolutionized the evaluation of rotational nystagmus by allowing detailed visualization of the structures involved in vestibular and ocular motor control:
Magnetic Resonance Imaging (MRI)
- High-Resolution Inner Ear Imaging:
- 3D-FLAIR sequences can visualize endolymphatic hydrops in Ménière’s disease
- High-resolution T2-weighted images show detailed anatomy of semicircular canals
- Gadolinium-enhanced sequences can identify inflammatory or neoplastic processes
- Brainstem and Cerebellar Imaging:
- Diffusion-weighted imaging (DWI) for acute stroke detection
- FLAIR sequences to identify demyelinating lesions
- Susceptibility-weighted imaging (SWI) for detecting microhemorrhages
- Specialized MRI Techniques:
- Diffusion tensor imaging (DTI) to assess white matter integrity
- Functional MRI (fMRI) to evaluate vestibular cortical processing
- MR angiography to assess vascular causes
Computed Tomography (CT)
While MRI is preferred for most soft tissue evaluation, CT imaging remains valuable for:
- Temporal Bone Assessment:
- High-resolution CT for detecting structural abnormalities of the inner ear
- Evaluation of superior semicircular canal dehiscence
- Assessment of temporal bone fractures
- Emergency Evaluation:
- Rapid assessment of intracranial hemorrhage
- Detection of hydrocephalus or mass effect
Advanced Vestibular Testing
- Video Head Impulse Testing (vHIT): This technique measures the vestibulo-ocular reflex for each semicircular canal individually, helping identify specific canal dysfunction that may contribute to rotational nystagmus.
- Rotational Chair Testing: Provides comprehensive assessment of horizontal canal function and can detect subtle vestibular asymmetries.
- Vestibular Evoked Myogenic Potentials (VEMP):
- Cervical VEMP (cVEMP) tests saccular function
- Ocular VEMP (oVEMP) tests utricular function
- Abnormal VEMP responses may correlate with rotational nystagmus patterns
Studies published in Frontiers in Neurology demonstrate that combining advanced imaging with specialized vestibular testing significantly improves diagnostic accuracy and helps guide targeted treatment approaches.
Treating Rotational Nystagmus: Multidisciplinary Approaches
Effective management of rotational nystagmus requires a comprehensive approach addressing both the underlying cause and symptomatic relief:
Cause-Specific Treatments
- BPPV Management:
- Canalith Repositioning Procedures: The Epley maneuver for posterior canal BPPV and Barbecue roll maneuver for horizontal canal BPPV
- Vestibular Rehabilitation: Customized exercises to promote central compensation
- Surgical Options: Posterior canal plugging for refractory cases
- Vestibular Neuritis Treatment:
- Corticosteroids: Early treatment with prednisone may improve recovery
- Vestibular Suppressants: Short-term use of meclizine or diazepam for acute symptoms
- Gradual Activity Resumption: To promote vestibular compensation
- Ménière’s Disease Management:
- Dietary Modifications: Low-sodium diet and diuretics
- Medications: Betahistine in some countries, intratympanic steroid injections
- Surgical Options: Endolymphatic sac decompression or vestibular nerve section for refractory cases
Symptomatic Treatments
- Pharmacological Interventions:
- Antihistamines: Meclizine, dimenhydrinate for acute symptom relief
- Benzodiazepines: Clonazepam or diazepam for severe acute episodes
- Antiemetics: Ondansetron or promethazine for associated nausea
- Newer Agents: 4-aminopyridine has shown promise in some forms of central nystagmus
- Optical Corrections:
- Prism Glasses: May help redirect visual input to reduce symptoms
- Tinted Lenses: Can reduce photophobia often associated with rotational nystagmus
- Contact Lenses: May provide proprioceptive feedback to help stabilize eye movements
- Physical Rehabilitation:
- Vestibular Rehabilitation Therapy (VRT): Customized exercises targeting specific deficits
- Balance Training: To reduce fall risk and improve functional mobility
- Gaze Stabilization Exercises: Help patients maintain visual focus during head movements
Innovative Treatment Approaches
- Virtual Reality Therapy: Emerging research suggests that controlled virtual reality environments may help retrain the vestibular system and reduce rotational nystagmus symptoms.
- Transcranial Stimulation: Studies are investigating whether transcranial direct current stimulation (tDCS) targeting vestibular cortical areas might modulate nystagmus patterns.
- Biofeedback Training: Some patients benefit from auditory biofeedback systems that provide real-time information about eye movements, allowing for conscious control strategies.
- Surgical Innovations:
- Minimally invasive approaches to semicircular canal plugging
- Improved techniques for vestibular nerve section
- Novel approaches to cerebellar stimulation
Adapting Your Environment for Rotational Nystagmus
Living with rotational nystagmus requires thoughtful environmental modifications to optimize function and safety:
Home Environment Adaptations
- Lighting Optimization:
- Uniform, glare-free lighting throughout living spaces
- Avoidance of flickering lights or strong contrasts
- Night lights for safe navigation in darkness
- Visual Stabilization Strategies:
- Reduction of busy visual patterns that may exacerbate symptoms
- Use of high-contrast markings for stairs and edges
- Strategic placement of visual anchors to aid orientation
- Safety Modifications:
- Installation of grab bars in bathrooms and stairways
- Removal of trip hazards like loose rugs
- Non-slip surfaces in wet areas
Workplace Accommodations
- Computer Work Adaptations:
- Larger monitors with adjustable height and angle
- Anti-glare screens and appropriate lighting
- Frequent breaks to reduce visual fatigue
- Meeting and Travel Considerations:
- Preferred seating positions to optimize visual stability
- Accommodations for motion sensitivity
- Modified travel policies when symptoms are severe
Transportation and Mobility
- Driving Considerations: Many patients with rotational nystagmus experience driving difficulties and may require:
- Formal driving evaluations by occupational therapists
- Possible restrictions on driving conditions (daylight only, familiar routes)
- Alternative transportation arrangements
- Public Transportation Strategies:
- Seat selection to minimize motion exposure
- Use of motion sickness medications when appropriate
- Planning for rest periods during long journeys
Research from Disability and Rehabilitation emphasizes that comprehensive environmental modifications, combined with appropriate medical treatment, can significantly improve quality of life for individuals with rotational nystagmus.
Patient Stories: Overcoming the Challenges of Rotational Nystagmus
Case Study 1: Recovery from Vestibular Neuritis
Sarah, a 42-year-old teacher, developed sudden onset rotational nystagmus following a viral illness. Initially debilitating vertigo and visual disturbance left her unable to work or drive. Through a combination of corticosteroid treatment, vestibular rehabilitation therapy, and gradual activity progression, she returned to full function within six months. Her key success factors included:
- Early recognition and treatment of vestibular neuritis
- Consistent participation in vestibular rehabilitation
- Gradual return to activities with appropriate modifications
- Strong family support and understanding from her employer
Case Study 2: Managing Chronic Ménière’s Disease
Robert, a 58-year-old engineer, experienced episodic rotational nystagmus as part of Ménière’s disease. His approach to management included:
- Dietary modifications with strict sodium restriction
- Prophylactic medications during high-stress periods
- Workplace accommodations including modified travel requirements
- Regular monitoring with an otolaryngologist
While not cured, Robert has successfully managed his condition for over five years with only occasional mild episodes.
Case Study 3: Pediatric Central Nystagmus
Eight-year-old Emma was diagnosed with rotational nystagmus secondary to a posterior fossa tumor. Following successful surgical resection and rehabilitation, she has adapted well with:
- Educational accommodations including preferred seating and extended time for visual tasks
- Regular occupational therapy focusing on visual-motor skills
- Family education about activity modifications and safety precautions
- Ongoing monitoring for residual effects
These cases illustrate the importance of individualized treatment approaches and the potential for good outcomes with appropriate management, even in challenging situations.
Conclusion: Navigating the Complexity of Rotational Nystagmus
Rotational nystagmus represents one of the most complex forms of involuntary eye movement disorders, requiring sophisticated diagnostic evaluation and multidisciplinary management. The circular nature of these eye movements often provides crucial diagnostic information about underlying vestibular and neurological pathology, making accurate recognition and interpretation essential for optimal patient care.
Recent advances in diagnostic imaging, vestibular testing, and treatment approaches have significantly improved outcomes for patients with rotational nystagmus. The development of targeted therapies, combined with improved understanding of the underlying mechanisms, offers hope for even better treatments in the future.
The key to successful management lies in:
- Prompt Recognition: Early identification of rotational nystagmus patterns and their diagnostic significance
- Comprehensive Evaluation: Thorough investigation to identify underlying causes
- Individualized Treatment: Tailored approaches addressing both specific pathology and functional needs
- Multidisciplinary Care: Coordination between neurology, otolaryngology, ophthalmology, and rehabilitation specialists
- Patient Education: Helping patients and families understand the condition and adapt effectively
For individuals experiencing symptoms suggestive of rotational nystagmus, consultation with a neuro-otologist or neuro-ophthalmologist is essential for proper evaluation and management. The complex nature of this condition requires specialized expertise to ensure accurate diagnosis and optimal treatment outcomes.
Understanding the relationship between rotational nystagmus and related conditions such as torsional nystagmus can provide additional insights into the spectrum of rotational eye movement disorders. Additionally, familiarity with comprehensive diagnostic testing approaches ensures thorough evaluation and appropriate treatment planning.
As our understanding of vestibular and ocular motor physiology continues to advance, new therapeutic options are likely to emerge, offering hope for improved outcomes and quality of life for patients affected by rotational nystagmus.
This article represents current medical understanding of rotational nystagmus based on peer-reviewed research and clinical guidelines. Individual cases may vary significantly, and this information should complement, not replace, personalized medical advice from qualified healthcare professionals specializing in vestibular and ocular motor disorders.