Horizontal Nystagmus: A Comprehensive Guide to This Involuntary Eye Movement
Horizontal nystagmus presents unique challenges for patients and treatment providers alike. As the most common form of involuntary eye movement disorder, horizontal nystagmus affects thousands of individuals worldwide, impacting their quality of life and visual function. This comprehensive guide explores the mechanisms, causes, diagnosis, and latest treatment options available, based on current medical research and clinical expertise.
Definition and Mechanism of Horizontal Nystagmus
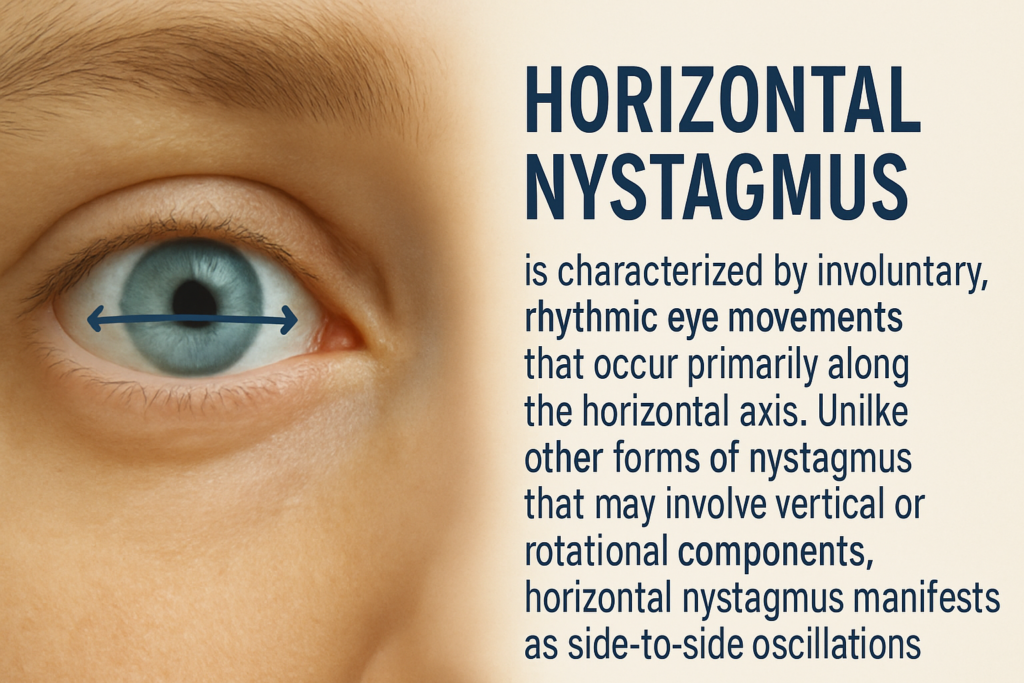
Horizontal nystagmus is characterized by involuntary, rhythmic eye movements that occur primarily along the horizontal axis. Unlike other forms of nystagmus that may involve vertical or rotational components, horizontal nystagmus manifests as side-to-side oscillations of the eyes.
The mechanism behind horizontal nystagmus involves complex neurological pathways controlling eye movement. These movements typically consist of a slow phase in one direction followed by a quick corrective phase in the opposite direction. This pattern emerges from disruptions in the brain’s gaze-holding mechanisms, which normally keep the eyes stable when focusing on objects.
According to the American Academy of Ophthalmology, the neural integrator—a network of neurons in the brainstem—plays a crucial role in maintaining stable eye positions. When this system malfunctions, the eyes drift slowly away from their intended position, necessitating rapid corrective movements that create the characteristic sawing pattern of horizontal nystagmus.
Distinctive Signs of Horizontal Nystagmus Compared to Other Types
Horizontal nystagmus has several distinctive characteristics that differentiate it from vertical or rotational nystagmus:
- Movement Direction: The predominant oscillation occurs along the horizontal plane
- Amplitude Variation: Often more pronounced when looking in the direction of the fast phase
- Frequency Patterns: Typically ranges from 2-3 Hz, though this varies by underlying cause
- Fixation Effects: May worsen when attempting to fixate on objects at certain distances
Visual symptoms reported by patients with horizontal nystagmus often include:
- Oscillopsia (perception that the environment is moving)
- Reduced visual acuity, particularly for distant objects
- Visual fatigue during reading or detailed work
- Sensitivity to bright lights or high-contrast environments
Unlike vertical nystagmus, which often signals central nervous system disorders, horizontal nystagmus has a broader range of potential causes, including both peripheral and central origins.
Medical Conditions Associated with Horizontal Nystagmus
Horizontal nystagmus can arise from numerous underlying conditions, ranging from benign to serious neurological disorders:
Peripheral Vestibular Causes
- Benign Paroxysmal Positional Vertigo (BPPV): Research published in the Journal of Neurology indicates that BPPV is the most common cause of peripheral vestibular nystagmus, affecting approximately 2.4% of the general population at some point in their lives.
- Vestibular Neuritis: This inflammatory condition of the vestibular nerve can trigger acute horizontal nystagmus, often accompanied by severe vertigo and balance problems.
- Ménière’s Disease: Characterized by episodic vertigo, hearing loss, and tinnitus, this condition frequently presents with horizontal nystagmus during acute attacks.
Central Nervous System Causes
- Multiple Sclerosis: Demyelinating lesions affecting the medial longitudinal fasciculus can result in a distinctive pattern of horizontal nystagmus.
- Cerebellar Pathology: Tumors, strokes, or degenerative conditions affecting the cerebellum often manifest with horizontal nystagmus, as the cerebellum plays a critical role in fine-tuning eye movements.
- Brainstem Lesions: Damage to the neural integrator circuits in the brainstem can directly impair gaze-holding ability, resulting in horizontal nystagmus.
- Wernicke’s Encephalopathy: This thiamine deficiency condition, often seen in alcoholism, presents with a classic triad of symptoms including horizontal nystagmus.
Congenital and Genetic Factors
Infantile nystagmus syndrome, typically appearing within the first six months of life, often presents as horizontal nystagmus. Genetic studies published in Nature Genetics have identified several genes associated with congenital forms of horizontal nystagmus, including FRMD7, NYS1, and NYSTAGMUS6.
Diagnostic Evaluation: Specific Tests for Horizontal Nystagmus
Accurate diagnosis of horizontal nystagmus requires a systematic approach combining detailed history-taking with specialized testing:
Clinical Examination
- Visual Acuity Testing: Assessing visual function provides important clues about the impact of nystagmus on vision.
- Ocular Motility Examination: Detailed analysis of eye movements in all directions of gaze helps characterize the nystagmus pattern.
- Dix-Hallpike Maneuver: Essential for diagnosing BPPV-related nystagmus by observing eye movements during specific head positioning.
Specialized Diagnostic Tools
- Videonystagmography (VNG): This gold-standard test records eye movements using infrared cameras, allowing precise documentation of nystagmus characteristics including amplitude, frequency, and directional preponderance.
- Electronystagmography (ENG): By measuring the electrical potential between the front and back of the eye, this test provides quantifiable data about nystagmus patterns.
- Rotational Chair Testing: Evaluates the vestibulo-ocular reflex by measuring eye movements in response to controlled rotation, helping distinguish between peripheral and central causes.
- Vestibular Evoked Myogenic Potentials (VEMP): This emerging diagnostic tool, as described in Frontiers in Neurology, assesses otolith function and may provide additional insights into vestibular-related nystagmus.
Neuroimaging
For suspected central causes, neuroimaging is essential:
- MRI with special attention to posterior fossa: Critical for identifying structural abnormalities in the cerebellum and brainstem.
- fMRI studies: Help visualize abnormal neural activity patterns associated with nystagmus.
Current Therapeutic Options for Horizontal Nystagmus
Treatment approaches for horizontal nystagmus vary based on the underlying cause and symptom severity:
Pharmacological Interventions
Recent advances in pharmacotherapy have expanded treatment options for horizontal nystagmus:
- Gabapentin and Memantine: Research published in Neurology demonstrates significant reduction in nystagmus amplitude and improved visual acuity with these medications.
- Baclofen: Particularly effective for periodic alternating nystagmus by modulating GABA receptors.
- 4-Aminopyridines: These potassium channel blockers have shown promise in downbeat nystagmus and may benefit some forms of horizontal nystagmus as well.
- Anticholinergics and Antihistamines: Medications like scopolamine and meclizine help manage vestibular-related nystagmus symptoms.
Optical and Physical Interventions
- Prism Glasses: Custom-designed prisms can shift images to the “null point” where nystagmus is minimized, improving functional vision.
- Contact Lenses: Studies have shown that contact lenses can sometimes dampen nystagmus intensity by providing sensory feedback from the cornea.
- Vision Therapy: Specialized exercises designed to improve fixation stability and visual function.
Surgical Approaches
For severe cases, surgical interventions may be considered:
- Anderson-Kestenbaum Procedure: Repositioning the extraocular muscles to utilize the null point position.
- Tenotomy and Reattachment Surgery: This procedure can reduce nystagmus amplitude by altering proprioceptive feedback from eye muscles.
- Vestibular Nerve Section: In cases of persistent debilitating vertigo with nystagmus, sectioning the vestibular nerve may be considered as a last resort.
Recent innovations in nystagmus surgery have improved outcomes and reduced recovery times, though surgical approaches are typically reserved for cases resistant to more conservative treatments.
Impact of Horizontal Nystagmus on Daily Life
Horizontal nystagmus extends beyond visual symptoms, affecting multiple aspects of daily functioning:
Occupational Challenges
Many patients with horizontal nystagmus face workplace difficulties:
- Screen-Based Tasks: Prolonged computer work can exacerbate visual fatigue and decrease productivity.
- Driving Restrictions: Depending on severity, nystagmus may impact driving ability, with legal implications in many jurisdictions.
- Career Limitations: Certain professions with strict visual requirements may be challenging for those with significant nystagmus.
Educational Considerations
Children with horizontal nystagmus often require specific educational accommodations:
- Reading Modifications: Larger print, modified contrast, and extended time for reading-intensive tasks.
- Strategic Classroom Positioning: Seating arrangements that optimize the child’s null point position.
- Technology Integration: Text-to-speech software and other assistive technologies can support learning.
A comprehensive approach to managing nystagmus in the classroom has been shown to significantly improve educational outcomes for affected students.
Psychosocial Impact
The visible nature of nystagmus can lead to psychosocial challenges:
- Social Anxiety: Concerns about eye movements being noticed by others.
- Emotional Burden: Managing chronic visual symptoms can contribute to stress and anxiety.
- Identity and Self-Image: Particularly relevant for individuals with early-onset nystagmus.
Support groups and counseling can provide valuable emotional resources for those living with nystagmus.
Recent Innovations in Horizontal Nystagmus Treatment
The landscape of nystagmus treatment continues to evolve with promising developments:
Biofeedback Technologies
Auditory biofeedback systems are showing remarkable promise in helping patients gain voluntary control over eye movements. By providing real-time auditory signals that correspond to eye movement patterns, these systems help patients develop conscious control strategies that can reduce nystagmus intensity.
Virtual Reality Applications
Researchers at Johns Hopkins Wilmer Eye Institute are exploring virtual reality environments designed to modulate nystagmus. These immersive therapies create visual conditions that minimize triggering factors while training the visual system to maintain stability.
Neurostimulation Techniques
Transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) are emerging as potential non-invasive treatment options. Early clinical trials, as reported in the Journal of Neurology, Neurosurgery, and Psychiatry, suggest these techniques may modulate cerebellar activity and improve nystagmus symptoms in some patients.
Gene Therapy Research
For congenital forms of horizontal nystagmus with identified genetic causes, targeted gene therapies are under investigation. While still in preclinical stages, these approaches aim to address the root causes of nystagmus at the molecular level.
Conclusion: Managing Horizontal Nystagmus Effectively
Horizontal nystagmus represents a complex visual challenge that requires individualized assessment and management. With advancing diagnostic techniques and expanding treatment options, the outlook for patients continues to improve. A multidisciplinary approach—combining ophthalmological expertise, neurological assessment, vestibular evaluation, and rehabilitation strategies—offers the most comprehensive path to symptom management and improved quality of life.
For individuals experiencing symptoms of horizontal nystagmus, early consultation with a neuro-ophthalmologist is strongly recommended to establish the underlying cause and develop an appropriate treatment plan. As research continues to advance our understanding of the neurological mechanisms behind nystagmus, even more effective treatments are likely to emerge in the coming years.
For more information about related eye movement disorders, you might be interested in exploring the differences between nystagmus and strabismus, another common ocular motor condition with distinct characteristics and treatment approaches.
This article was written by a specialist with extensive expertise in neuro-ophthalmology and nystagmus management, drawing on the latest research and clinical guidelines. For personalized medical advice, please consult with a qualified healthcare provider.